Pericardial effusion (fluid around the heart) can be caused by many different disease processes, including neoplasia/cancer, bleeding disorders, heart failure, systemic inflammatory or infectious disease, and kidney failure. In some cases, no identifiable cause is found (idiopathic effusion). The most common causes of pericardial effusion in dogs are neoplasia and idiopathic effusion.
Regardless of the cause, pericardial effusion can become life-threatening as it can increase the pressure within the pericardial space causing compression of the heart (cardiac tamponade). When this occurs, blood flow to the lungs and the rest of the body is diminished causing clinical signs of exercise intolerance, collapse/syncope, cyanosis (blue mucous membranes), difficulty breathing, and death from respiratory or cardiac arrest. Blood returning to the heart begins to pool leading to leakage of fluid into the space around the lungs (pleural effusion) or the abdomen (ascites) in some cases. This can result in abdominal distension and further difficulty in breathing. Pericardial effusion can also cause life-threatening arrhythmia (abnormal heartbeats).
The diagnostic work-up for patients with pericardial effusion often includes echocardiography, abdominal ultrasound, bloodwork, ECG, thoracic radiographs, pericardial fluid analysis, coagulation tests, and troponin assessment. Specific diagnostics tests are chosen based on history and breed as not all of these tests are necessary for every patient.
Treatment
Treatment ultimately depends on the underlying cause of the effusion. For idiopathic effusions, some patients never have a second episode while others have recurrent effusions requiring medical and/or surgical intervention. In cases of recurrent idiopathic effusions and some types of cancer, surgical removal of the pericardium (called pericardectomy) is recommended to prevent life-threatening complications of pericardial effusion. For effusions caused by cancer, chemotherapy and radiation are sometimes recommended to shrink the size of the tumor and mitigate the chance of future bleeding/effusion.
In many cases, echocardiography is unable to identify a mass/tumor in the early stages of the disease. Regardless of the cause, effusions can recur at any time. Supplements (Yunnan Baiyao and I’mYunity®) and medications (tranexamic acid or aminocaproic acid) are sometimes recommended to mitigate the risk of recurrent effusion; some of these may also slow the progression of some tumor types.
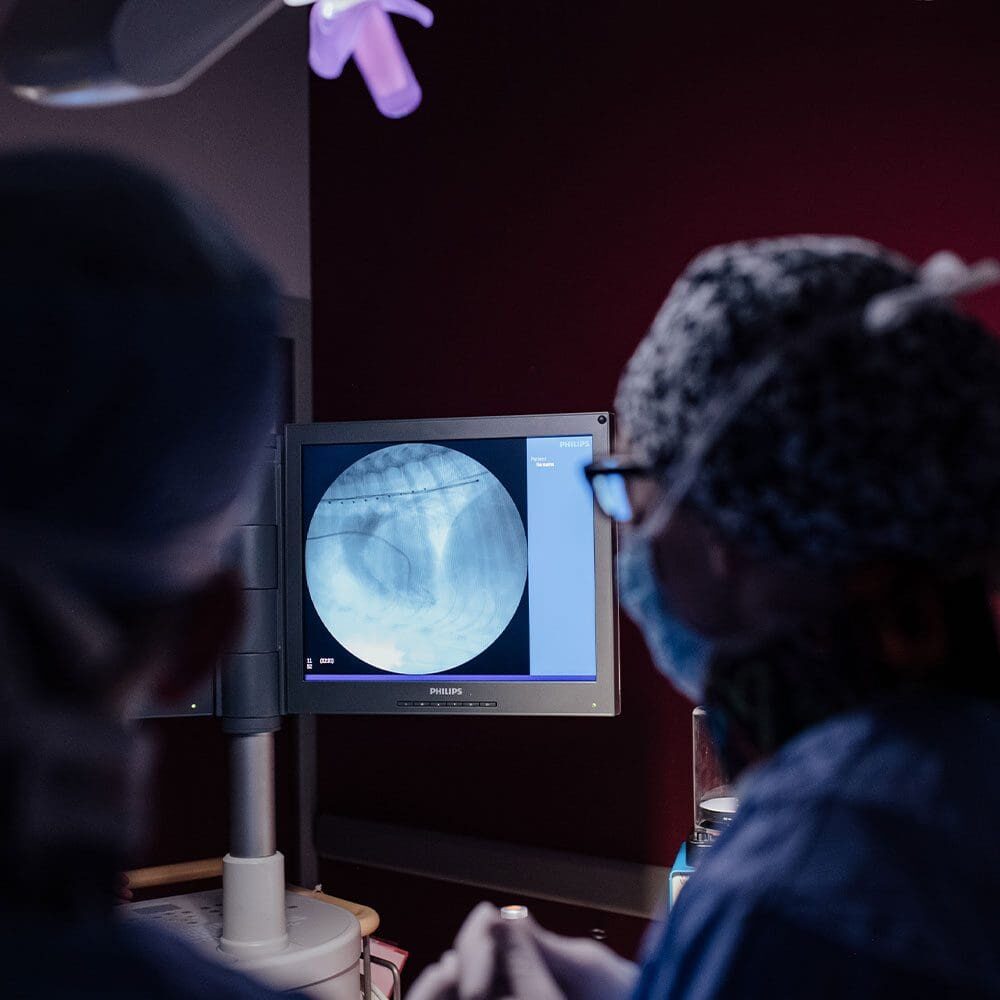
When cardiac tamponade is present, a procedure to remove the fluid from the pericardial space is performed urgently (called pericardiocentesis). This procedure requires the insertion of a needle/catheter into the pericardial sac. The fluid removed can be submitted to the lab for analysis (cytology), to screen for some of the causes of pericardial effusion.
Prognosis
The prognosis for patients with idiopathic pericardial effusion is often good/excellent; although some require surgical removal of the pericardium to achieve this favorable prognosis. For those patients with neoplasia/cancer, the prognosis depends largely on the type of cancer and the frequency of recurrence of pericardial effusion. The most common cancer associated with the heart is hemangiosarcoma (~70% of cases), which carries a grave prognosis with a median survival time of 2-3 months without further treatment.
With chemotherapy and surgical removal (for select cases), the median survival time increases to about 4-6 months. The second most common type of cancer associated with the heart is chemodectoma. These tumors are common in Bulldogs, Boston Terriers, and other short-nosed breeds. Chemodectomas tend to be slow-growing and do not readily metastasize providing a more favorable prognosis. Overall, the median time for a patient to have a recurrence of pericardial effusion is 10 days, however, this is highly variable. Unfortunately, those patients who have ventricular arrhythmia as a result of their disease are at risk of experiencing sudden cardiac death.

