Radiation therapy is a treatment modality that has the capability of controlling, curing or palliating certain types of cancer. Veterinary Specialty Center is proud to be one of only a few facilities in the Chicagoland area to provide radiation therapy as an option for companion animals with cancer or severe inflammatory conditions. This handout is designed to provide an introduction to the use of radiation therapy in companion animals. It is not designed to replace consultation with your pet’s veterinary team.
What is radiation therapy?
Radiation therapy is the use of high-energy x-rays or electrons in the fight against cancer. Your pet is not radioactive during the treatment course.

How is radiation therapy given?
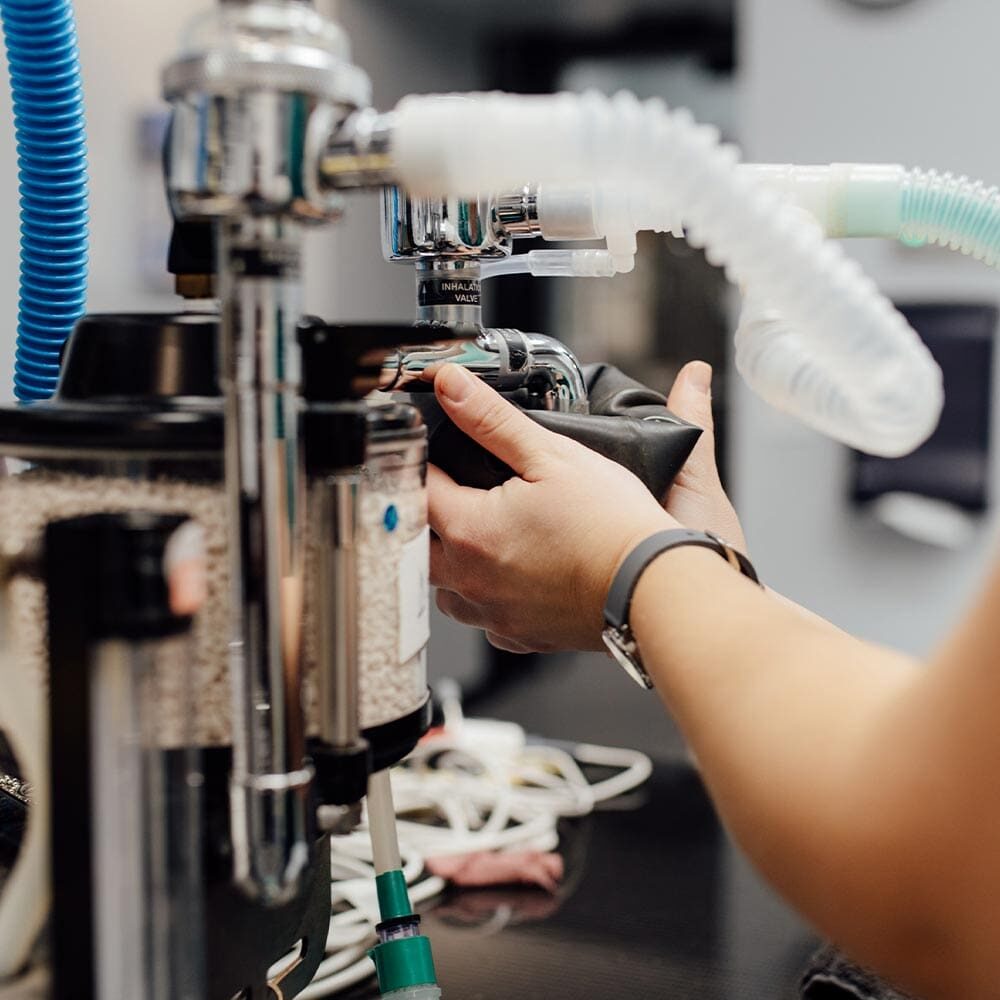
The machine utilized to produce the X-rays for radiation therapy is called a linear accelerator (LINAC). The LINAC is housed in a special room designed to protect the surrounding environment and operators from the energy of the X-ray beam. The radiation delivered is much higher (1,000 X) than the radiation used to generate images (diagnostic X-rays), which is why it is highly destructive to cancer cells.
The total radiation dose is prescribed for the patient by the radiation oncologist. The total radiation dose is not given all at once but is subdivided into “fractions”, or individual treatments. A single fraction is most commonly given daily, but sometimes twice a day at least 6 hours apart. Therapeutic radiation is delivered this way because over many days a large dose of radiation is delivered to the cancer cells, while the normal tissues have 24 hours (or several days) in between each fraction to heal from radiation-induced damages. Cancer cells are not as efficient at healing as normal, healthy tissue, which is why they are preferentially affected and killed. The number of fractions required is dependent on individual patient requirements.
During the first day of radiation therapy, the patient is anesthetized and positioned. Special laser positioning tools are used to ensure that the prescribed dose is given to an accurate area on the patient. Often, patients receive skin markings, which allow subsequent treatments to be given to an identical area. The first treatment may take 1-2 hours depending on the complexity of the treatment plan. Subsequent fractions are scheduled based on the treatment plan. Thee fractions require general anesthesia to immobilize and properly position the patient, requiring a breathing tube (i.e. endotracheal tube). Each subsequent fraction requires 30-40 minutes to complete on average, but may be as short as 15 minutes or as long as 90 minutes. If advanced imaging and computer planning are needed or recommended to treat a tumor, a CT scan is required prior to starting radiation therapy. Most computer radiation plans can be completed in 2-5 business days, but the timeline depends on the complexity of the treatment.
What are the side effects of radiation therapy?
Side effects of radiation therapy are usually related to local inflammation of the tissues incorporated into the radiation therapy field. If the tumor being treated is, or was, on the skin, side effects may include skin redness, moist eczema, itchiness, and localized hair loss. These effects are DELAYED and may take several days to 2-3 weeks before they are seen. The time to resolution of these side effects varies, ranging from never occurring to subsiding in 3 to 4 weeks after completing therapy. Regrowth of hair may take months. Hair may regrow in a different color or in some cases may not regrow at the radiation site. Occasionally organs that are adjacent to the radiated field may have some complications. This can be anticipated and discussed after the radiation plan is formulated.
What is the cost of
radiation therapy?
What is the cost of radiation therapy?
Radiation therapy involves a large amount of state-of-the-art equipment and personnel with years of training to plan and administer the treatments. Therefore, radiation therapy is an expensive treatment modality. The exact cost is dependent on the type of tumor being treated and the complexity of the treatment plan.
What do I do next?
If your pet’s primary care physician has identified a tumor that is potentially treatable with radiation therapy, please call our office at (847) 459-7535 to schedule a consultation with our radiation oncologist. During this consultation, we will discuss the type of tumor your pet has, and give you some options for treatment of your pet.


What can I expect during the treatment course?
Hopefully, this information will help you better understand what to expect and make things a little less scary. If you have any questions at all, please ask. We are here to help you.

